Autoimmune Connective Tissue Disease
What is Autoimmune or Connective Tissue Disease-Related ILD?
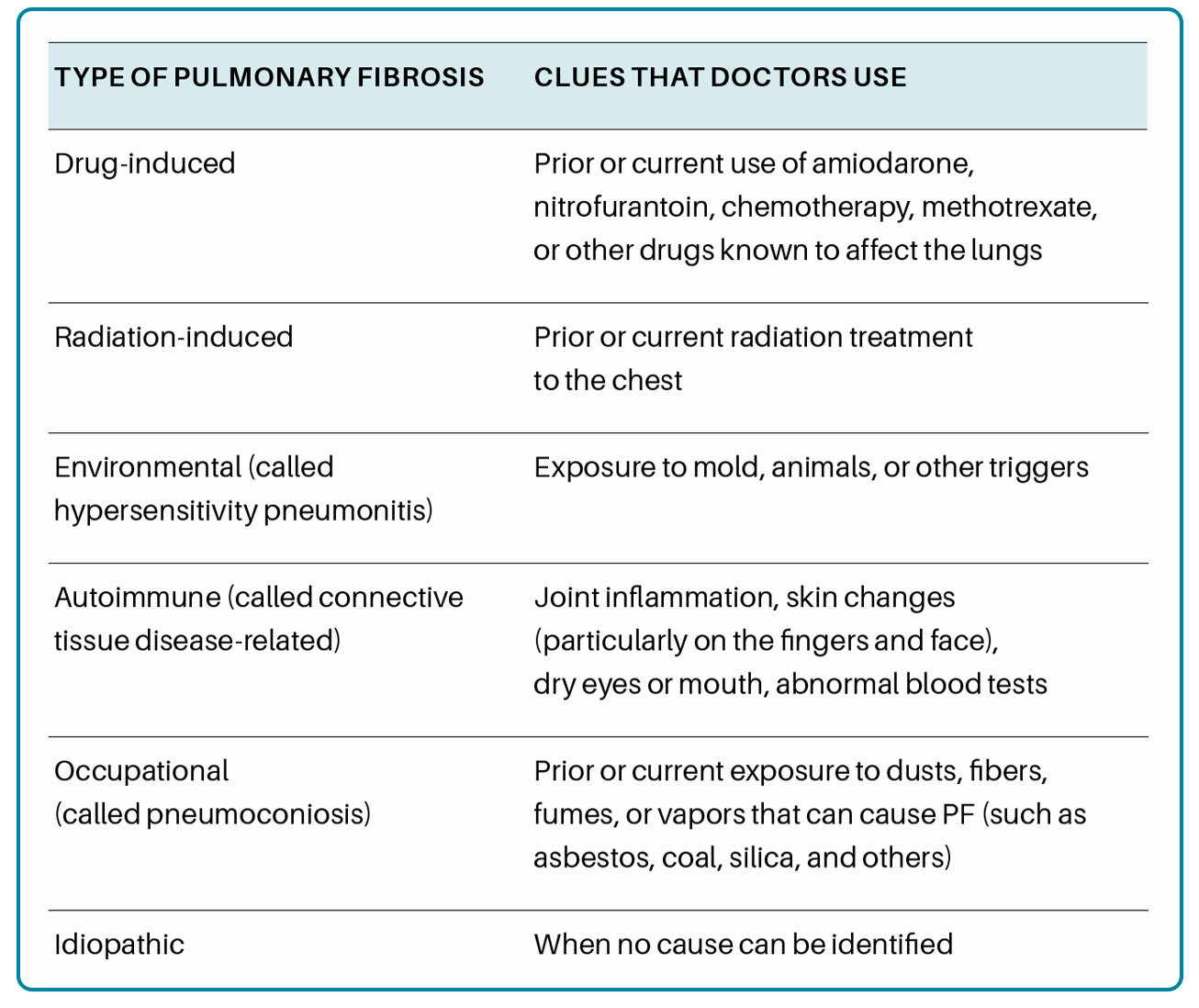
Pulmonary fibrosis (PF) is part of a larger group of more than 200 interstitial lung diseases (also known as ILDs) that are characterized by inflammation and/or scarring in the lung. In ILDs, the injury and damage occurs in the walls of the air sacs of the lung, as well as in the tissue and space around these air sacs. When an interstitial lung disease includes scar tissue in the lung, we call it pulmonary fibrosis.
Autoimmune diseases are also called connective tissue diseases, collagen vascular diseases, or rheumatologic diseases. “Auto” means self, and “immune” refers to your immune system. In autoimmune disease, the body’s immune system can attack its own organs, causing inflammation and injury. In some autoimmune diseases multiple organ systems can be involved, including the respiratory system. The inflammation and scarring in the lungs caused by an autoimmune condition is called autoimmune- or connective tissue disease-related interstitial lung disease (ILD).
Autoimmune diseases are a diverse group of diseases that have some similarities, but are also distinctly different from each other. Not all autoimmune conditions cause lung injury that can lead to scarring in the lungs, or pulmonary fibrosis. Even in autoimmune conditions that can cause lung injury, pulmonary fibrosis is not always present.
What are the Symptoms of Autoimmune-Related Pulmonary Fibrosis?
Early in the disease, people with autoimmune-related pulmonary fibrosis may not experience symptoms or might have a bothersome cough. As the disease progresses, breathlessness during exercise and daily activities can be common. Fatigue, depression, or anxiety are also commonly experienced by people living with autoimmune-related ILD. In some patients, respiratory symptoms may be the first sign that they have an autoimmune condition.


What Causes Autoimmune-Related ILD?
The body's immune system protects us from harmful substances like bacteria, viruses, allergens and toxins by producing antibodies to combat these substances. In an autoimmune condition, the body produces antibodies to an unknown trigger, and these antibodies attack healthy tissue in the body. In autoimmune-related ILD, these antibodies attack the lungs, causing inflammation and scarring. For some types of autoimmune conditions there may be risk factors that are related to the development of disease, such as genes that make a person more susceptible to developing autoimmune disease. However, in general, the cause of autoimmune-related ILD is not well understood. Read our Causes page for more information.
How Is Autoimmune Or Connective Tissue Disease-Related ILD Diagnosed?
When a doctor or other healthcare provider suspects that a patient has ILD, they will collect information about the patient’s medical and personal history, work and home environment, hobbies, and illness that may be present in the family. This can help a doctor identify exposures or other diseases that might have caused lung injury and scarring. The doctor will also often order pulmonary function tests, a chest x-ray, blood work, and a high-resolution CT scan. Read our Diagnosis page for more information.
Pulmonary function tests measure how much air the lungs can hold, and how the lungs are working overall. Scarring can cause the lungs to shrink, and it can also make them stiff and unable to fully expand. This means the lungs are able to hold less air. Scar tissue may also affect the ability of the lungs to transfer oxygen to the bloodstream.
A high-resolution computed tomography (HRCT) scan is a special type of x-ray that shows fine detail of the lung tissue. On a CT scan (also known as CAT scan) healthy lung tissue looks nearly black, and scar tissue and inflammation appear grey or white.
Blood tests can help to identify antibodies, proteins or other factors present in the blood that are specific to a particular autoimmune condition. The presence of these indicators may confirm a diagnosis of autoimmune disease. This information, in combination with a patient’s other symptoms and HRCT findings, may indicate the presence of an ILD that is associated with a patient’s autoimmune condition.
Diagnosing an ILD involves many different types of information, and when another disease is present, diagnosis can be complicated. In most cases, a pulmonologist will work with a rheumatologist, a doctor who specializes in autoimmune diseases, to establish a diagnosis of autoimmune-related ILD.


Rheumatoid Arthritis-Associated Interstitial Lung Disease (RA-ILD)
Rheumatoid arthritis (RA) primarily causes arthritis which affects the joints, but people living with RA can also develop lung disease, problems with the nerves, eyes, and other types of inflammation in the body. Many people with RA do not have lung disease. When RA does affect the lung, it can lead to many different lung conditions. ILD is the most common problem in the lungs of people living with RA. When doctors use the term RA-ILD, they are usually referring only to ILD involving the lungs in someone living with RA. Certain medications to treat RA can have side effects that involve the lung, including lung infections (due to a weakened immune system) and even ILD caused by the medications.
Systemic Sclerosis-Associated Interstitial Lung Disease (SSc-ILD)
People living with systemic sclerosis, sometimes called “scleroderma,” most commonly have thickening and tightening of the skin on the fingers and other parts of the body. Scleroderma can also affect the kidneys, GI tract (particularly the esophagus), and lungs. Many people with scleroderma do not have lung disease. When scleroderma does affect the lungs, it most frequently leads to one of two conditions: ILD or pulmonary hypertension (PH). Some people can have both ILD and PH. People taking certain medications to treat scleroderma can also develop lung infections, such as pneumonia.


Sjögren’s Syndrome
Sjögren’s syndrome is a disorder affecting the mucous membranes and moisture-secreting glands of the eyes and mouth. While the most common symptoms are dry eyes and dry mouth, people who have Sjögren’s syndrome may also experience joint problems, skin rashes, and fatigue. Sjögren’s syndrome can affect other systems of the body, including the lungs. In some patients, Sjögren’s syndrome can lead to interstitial lung disease. Sjögren’s syndrome can often accompany other autoimmune disorders.
Polymyositis, Dermatomyositis, and Antisynthetase Syndrome
Myositis diseases are autoimmune conditions that cause inflammation and damage to the muscles. Polymyositis and dermatomyositis can cause gradual development of weakness with associated difficulty swallowing, pain and weakness in the joints, and fatigue. ILD can develop in patients with polymyositis and dermatomyositis. People who have dermatomyositis also have a distinctive rash that can affect the upper part of their body, back, and joints. Women are twice as likely as men to be diagnosed with polymyositis and dermatomyositis.
People who have myositis may also be diagnosed with antisynthetase syndrome, which typically occurs in patients who have myositis in combination with specific autoantibodies, known as antisynthetase antibodies. In addition to symptoms associated with myositis disease, those diagnosed with antisynthetase syndrome can develop Reynaud’s disease, thickening and cracking of the skin on the hands, and fever that is not associated with infection. They are also more likely to develop ILD associated with their disease.


How Is Autoimmune-Related ILD Treated?
Treatment for ILD associated with an autoimmune condition may be specific to the autoimmune diagnosis that a patient has. In some cases, medications that weaken the immune system are used to treat inflammation in the lungs, which may be helpful in reducing lung injury. In some patients, doctors monitor the disease without medications. Treatments for symptoms associated with an autoimmune condition, such as joint inflammation, do not necessarily treat the associated lung disease. Patients who have ILD related to an autoimmune condition should also be treated by a rheumatologist.
Supplemental oxygen, pulmonary rehabilitation, and management of symptoms are important treatment options for many types of pulmonary fibrosis, and may also be appropriate for people who have autoimmune-associated ILD. Smoking cessation and routine vaccinations are important parts of living with pulmonary fibrosis. Lung transplantation may be an appropriate treatment for some people living with autoimmune-related ILD.
What Should I Do Next?
If you have been recently diagnosed with pulmonary fibrosis, consider making an appointment with a pulmonologist who has experience caring for patients with PF. A knowledgeable team of experts will help make sure you receive an accurate diagnosis and
the most up-to-date treatments and management recommendations. To assist you in finding pulmonologists nearest to your home who provide expert care to patients with PF, the Pulmonary Fibrosis Foundation established the PFF Care Center Network, which includes 68 medical centers throughout the United States. You can search for the PFF Care Center Network medical center closest to
you here.
We also recommend that you join a pulmonary fibrosis support group. Connecting with other individuals facing the same illness can help you and your family feel less alone in your journey with pulmonary fibrosis. Support groups can supplement the care
you receive from your healthcare team by providing emotional support and education. You can find a list of support groups
here.
Support groups can help those living with pulmonary fibrosis to:
- Learn about their disease and available treatments
- Feel supported by others who share similar experiences living with PF
- Learn to navigate the healthcare system more effectively
- Improve coping skills, connect with helpful resources, and more
Contact the PFF Help Center by calling 844.TalkPFF (844.825.5733) or email help@pulmonaryfibrosis.org. We can help answer your questions, discuss your concerns, and connect you with resources.

Educational Materials
Find reliable information and trusted resources that can help you learn about pulmonary fibrosis and live better with PF.
-
View Full Details
Pulmonary Fibrosis Information Guide
Our comprehensive guide provides reliable information about pulmonary fibrosis, the diagnostic process, treatment options, and more. -
View Full Details
Scleroderma-associated Interstitial Lung Disease (SSc-ILD) Fact Sheet
Scleroderma-associated interstitial lung disease is a chronic lung disease in which scar tissue and/or inflammation builds up in the walls of the air sacs of the lungs in a person with a diagnosis of scleroderma. Read this fact sheet for more information about this form of pulmonary fibrosis. -
View Full Details
Rheumatoid Arthritis-associated Interstitial Lung Disease (RA-ILD) Fact Sheet
Rheumatoid arthritis-associated interstitial lung disease is a chronic lung disease in which scar tissue and/or inflammation builds up in the walls of the air sacs of the lungs in a person with a diagnosis of rheumatoid arthritis. Read this fact sheet for more information about this form of pulmonary fibrosis.

PFF Help Center
For those living with pulmonary fibrosis, obtaining the most accurate and current information can be a frustrating and challenging task. Let us help you find your answers.