PFF Funded Research

A History of Funding Research
The PFF has been funding research since its inception in 2000. From the PFF Registry to the PFF Scholars and collaborative initiatives with governmental and industry partners, accelerating the path to a cure is a priority of the Foundation.
PFF Registry
The PFF Registry is a distinctive database that follows the care of patients with broadly defined interstitial lung diseases including idiopathic pulmonary fibrosis, connective tissue disease, hypersensitivity pneumonitis, and other diagnoses. The PFF Registry collects clinical and self-reported outcomes data from PF patients as well as lung transplant recipients with PF, family members, and caregivers.


PFF Scholars
In 2019, the PFF redefined its objectives for funding research and introduced the PFF Scholars program, which has replaced the established and junior investigator awards.
The PFF Scholars program focuses on engaging early-career investigators in their emerging research in the field of pulmonary fibrosis. With the goal of advancing research that could translate into successful therapies for PF, the PFF Scholars program is designed to support and enable promising researchers to obtain independent funding and continue their cutting- edge research.
Scholars will receive up to $100,000 over a two-year period and will be assigned a PFF Scholar Sponsor, who will actively advocate on behalf of the awardee and work to create opportunities for leadership, networking, and visibility in the field.
The Foundation’s Research Review Committee, which is comprised of a wide-ranging group of international experts, administers the peer-review process.
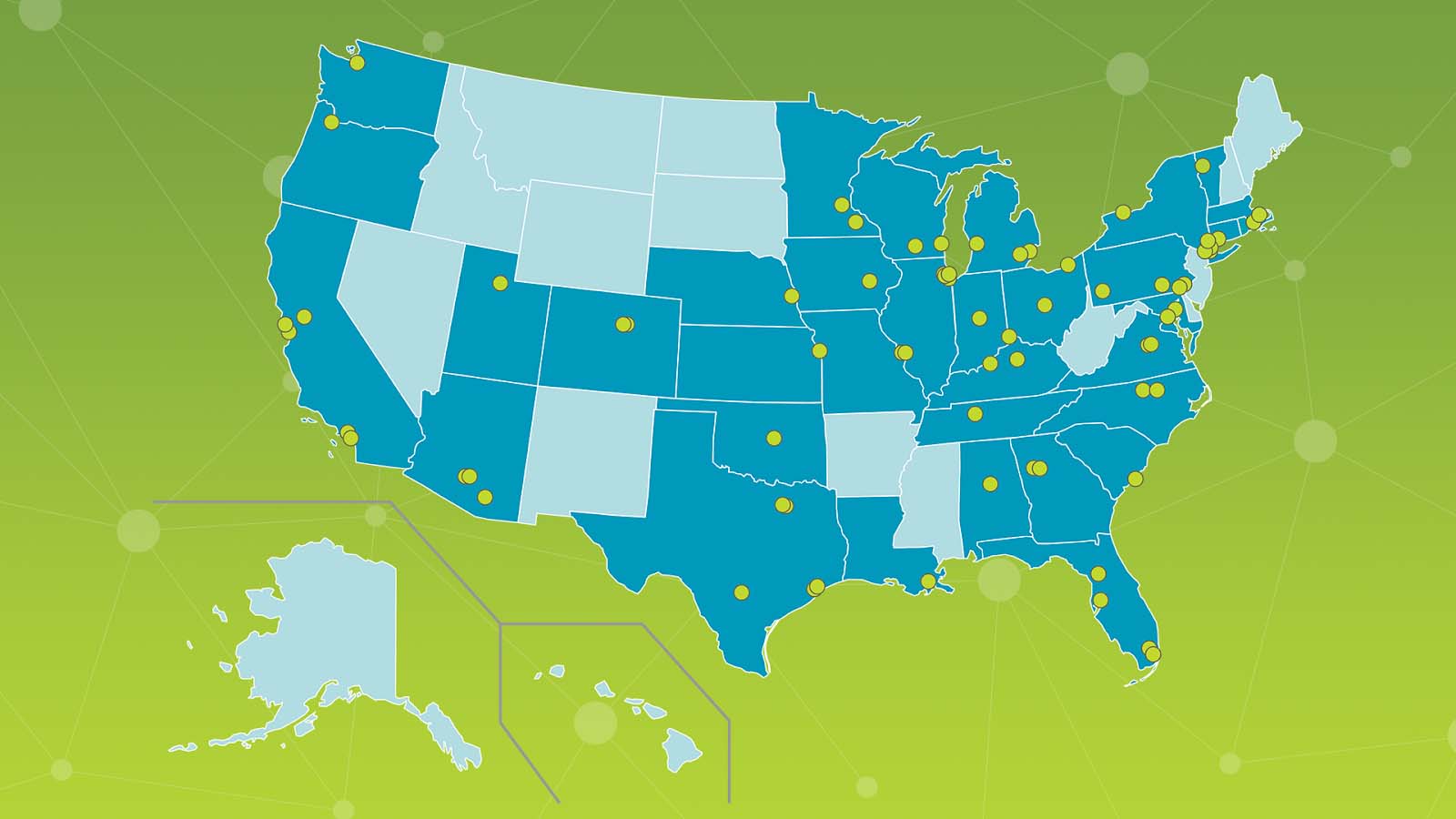
PFF Care Center Network
The
PFF Care Center Network is a growing group of 68 medical centers nationwide
that specialize in the diagnosis, care, and treatment of individuals living
with pulmonary fibrosis. Care Centers offer expert teams that work to improve
the lives of patients and their families. As participants in the Care Center
Network, medical centers actively engage their local PF communities in research
activities. This
enables us to enhance our understanding of PF and expedite efficient clinical
trials to identify effective therapies.
Collaborations
The PFF actively partners with various organizations to discover and advance new therapies to treat and cure disease. We aim to establish an environment to sustain continued and enhanced investment in PF treatments. One such collaboration is PROLIFIC, an industry consortium that could speed up the development of targeted treatments for IPF patients.