Maintain Your Health

Maintaining Your Health
While your doctors, nurses, and other care providers will help you to manage your disease, you are your most important advocate since you are the center of your treatment. People who take an active role in their own care frequently have better results in the long run.
There are a variety of things that you can do to maintain or improve your quality of life while living with pulmonary fibrosis. Below are steps you can take to maximize your care and maintain your health.
Speak up for Yourself
Remember you are a part of a healthcare team that includes your doctors and nurses. If you have any concerns with your treatment or do not understand something about your disease, it is essential that you talk to your care providers. They want to make sure that you are able to maintain your health and will assist you with these issues. You are your own best advocate.

Be Prepared for Your Visits
Being prepared goes a long way in communicating with your providers – you cannot assist in the decision making process if you do not understand the factors involved.
Your healthcare team will be asking you a lot of questions. As a member of that team, you have a responsibility to do your part. Be prepared to ask your own questions and participate. Prepare a list of your questions or concerns for your physician and bring it to your visit. Here is a list of questions for your doctor.
You will likely receive a significant amount of information during your health care visits and this can be overwhelming. Do not be afraid to take notes to help you remember important treatment issues later on. It may be helpful to bring someone with you to each appointment to help you take notes. The PFF Physician Notepad is a helpful tool to take notes during appointments and facilitate a conversation between you and your doctor.
Let Your Family and Friends Help
Emotional support is very important to maintaining your health. This is especially true if you are trying to modify your lifestyle. Quitting smoking, exercising more, or changing your diet is difficult; let those who care about you help you accomplish your goals. Do not be afraid to bring people who support you to your health appointments.


Join a Support Group and Help Others With PF
Reach out to community or national groups that assist people with pulmonary fibrosis. Just knowing that there is someone out there that knows how you feel is comforting. Share ideas, share fears, and share joys. It can be very useful to find out how other people manage their disease. They may give you invaluable tips or tools that make it easier to manage your health, and you can then pass your tips on to others to help support the community. You can search for PFF support groups.
Consider participating in the Pulmonary Fibrosis Foundation's advocacy program. You may gain strength in knowing that you are helping future patients and researchers by advocating for the pulmonary fibrosis community.
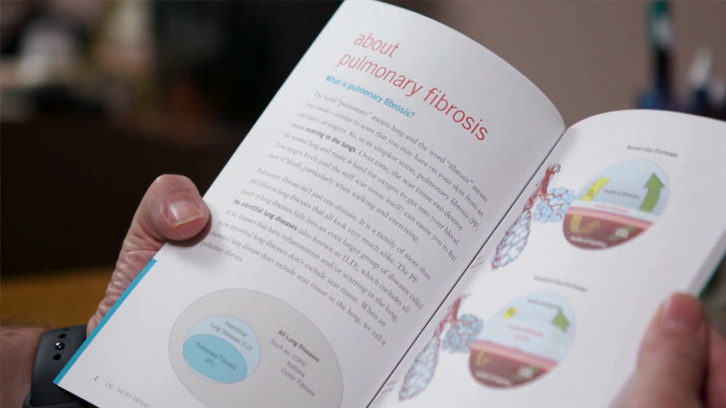
Stay Informed
Continue to learn about pulmonary fibrosis. The more you know, the better you will be able to manage your disease and recognize when you need to access health services. Be advised that there is misinformation on the internet; to ensure your safety, make sure you access reliable sources of information, such as advocacy groups and respected scientific and medical sources. You can access a full list of the PFF’s educational resources.

Stay in Shape
One of the most damaging consequences of lung disease and its sensation of breathlessness is the development of an inactive lifestyle. People with pulmonary fibrosis sometimes limit their physical activities in an attempt to avoid breathlessness. Regular exercise can strengthen your muscles and make them more resistant to fatigue. With practice and training you can learn to perform tasks in a more efficient manner. By being more efficient, you need less oxygen for the same amount of work. The result is that you may find that you have more energy to accomplish daily tasks and that you are less short of breath. A formal rehabilitation program called pulmonary rehabilitation is preferred because it allows for observation during exercise and it can be tailored to your specific needs.
Eat Well and Get Plenty of Rest
Getting at least eight hours of sleep every night can boost your immune system and sense of well-being.


Stop Tobacco Use
Take Steps to Prevent Respiratory Infections
- Get a flu vaccine every year. Everyone older than six months of age in the home needs to be vaccinated against influenza every year.
- Make sure you have received a pneumonia vaccine if you are over age 65. Younger adults with certain health conditions may also need to be vaccinated against pneumonia.
- Get vaccinated for COVID-19.
- Wash your hands or use hand sanitizer frequently, especially after returning home.
- Notify your primary care provider immediately at the onset of a cold, cough, or flu.
- Avoid large crowds.
- Know when to say NO to visits from family or friends; to sitting in a hospital emergency waiting room with sick people; or anything else you feel is unsafe. You are the best judge of what is okay or not.


Practice Relaxation Techniques and Keep a Positive Attitude
Learning relaxation techniques can help you manage the anxiety that often accompanies breathlessness. Joining a support group and/or seeing a counselor can help you cope with your feelings and the anxiety and depression that are common in people with pulmonary fibrosis. The restriction on activity due to shortness of breath may lead to isolating oneself from family and friends, adding to the depression.
Actively participating in the management of your disease is greatly enhanced by a positive attitude. A positive attitude can help you and your loved ones cope with the disease.
Prepare for the Future
Learn about Advance Directives (Living Wills & Medical Power of Attorney), Physician Orders for Life-Sustaining Therapy (POLST), and palliative care options, even long before they seem to be needed. These documents should be kept in a place where they are easy for you to find. You can also add copies to your medical record at the clinic where you receive care.
It's important to select a person to be your decision maker when you are no longer able to make decisions, and make that person aware of your wishes so that they can honor those wishes.


Learn about Quality of Life Care
Palliative Care: Using a multidisciplinary approach, palliative care can involve physical, psychosocial, and spiritual factors in the treatment approach. Teams may include physicians, pharmacists, nurses, religious leaders, social workers, psychologists, and other health care professionals. These teams focus on concrete goals including relief from breathlessness and other distressing symptoms, spiritual care, development of support systems, and encouraging an active lifestyle.
Hospice Care: Hospice care is a type of end-of-life care, intended to help people who are dying find peace, comfort, and dignity. It is generally reserved for those who have less than six months to live and often includes treatments to control breathlessness and other symptoms to maintain comfort. Hospice care also provides support to families. Care can be provided at a hospice center but can also be done in nursing facilities, hospitals, or at home.
FAQs
Acknowledgments
Educational Materials
Find reliable information and trusted resources that can help you learn about pulmonary fibrosis and live better with PF.
-
View Full Details
Pulmonary Fibrosis Quick Facts
This one-page document provides quick facts about pulmonary fibrosis, including symptoms, causes, treatment options, and more. -
View Full Details
Pulmonary Fibrosis Information Guide
Our comprehensive guide provides reliable information about pulmonary fibrosis, the diagnostic process, treatment options, and more.

PFF Help Center
For those living with pulmonary fibrosis, obtaining the most accurate and current information can be a frustrating and challenging task. Let us help you find your answers.